Published: 02/13/2025
By Melanie Kiener, Assistant Professorof Infectious Diseases. Baylor College of Medicine and Desiree LaBeaud, Professor of Pediatric Infectious Diseases. Stanford University
The ongoing pandemic of antimicrobial resistance (AMR) poses a severe threat to human health. In 2019, it resulted in an estimated 1.27 million global deaths due to the inability to treat infections and contributed to another 4.95 million deaths (1). The highest rates of AMR are seen in low- and middle-income countries (LMICs). While there are many different factors that contribute to AMR, including antibiotic use in the food supply and ability to buy antibiotics without a prescription, the overuse and misuse in the healthcare setting is also an important contributor. Frequent antibiotic use can lead to resistant bacteria, meaning infections will be harder to treat, with higher associated morbidity and mortality.
In our study, recently published in PLOS Global Public Health, we aimed to describe factors associated with antibiotic prescribing at outpatient clinics in Kenya in children and adults. Clinicians here have access to rapid malaria testing, but otherwise point of care diagnostics in these resource limited settings are not routinely available. We examined over 1,500 sick visit encounters between 2019 and 2022 and found that antibiotics were prescribed in nearly three-fourths of encounters, despite only about half of them with a clinician reported diagnosis that would warrant an antibiotic. In children less than 5 years, over 80% received an antibiotic. Those who were younger, had negative malaria tests, and cardiac or respiratory symptoms were prescribed antibiotics more often. We also found that visits taking place after the start of the COVID-19 pandemic were also more likely to result in an antibiotic prescription compared to visits before, which is a trend that was seen globally during the early pandemic.
Our results show a high number of unnecessary antibiotic prescriptions and highlight the need for improved access to point of care diagnostics in low-resource clinical settings to rule in viral infections. Additionally, antimicrobial stewardship programs targeted to outpatient LMIC clinicians are needed to train clinicians on safe and appropriate uses of antibiotics to decrease rates of resistant infections in the community.
Reference: Antimicrobial Resistance Collaborators. (2022). Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet; 399(10325): P629-655. DOI: https://doi.org/10.1016/S0140-6736(21)02724-0
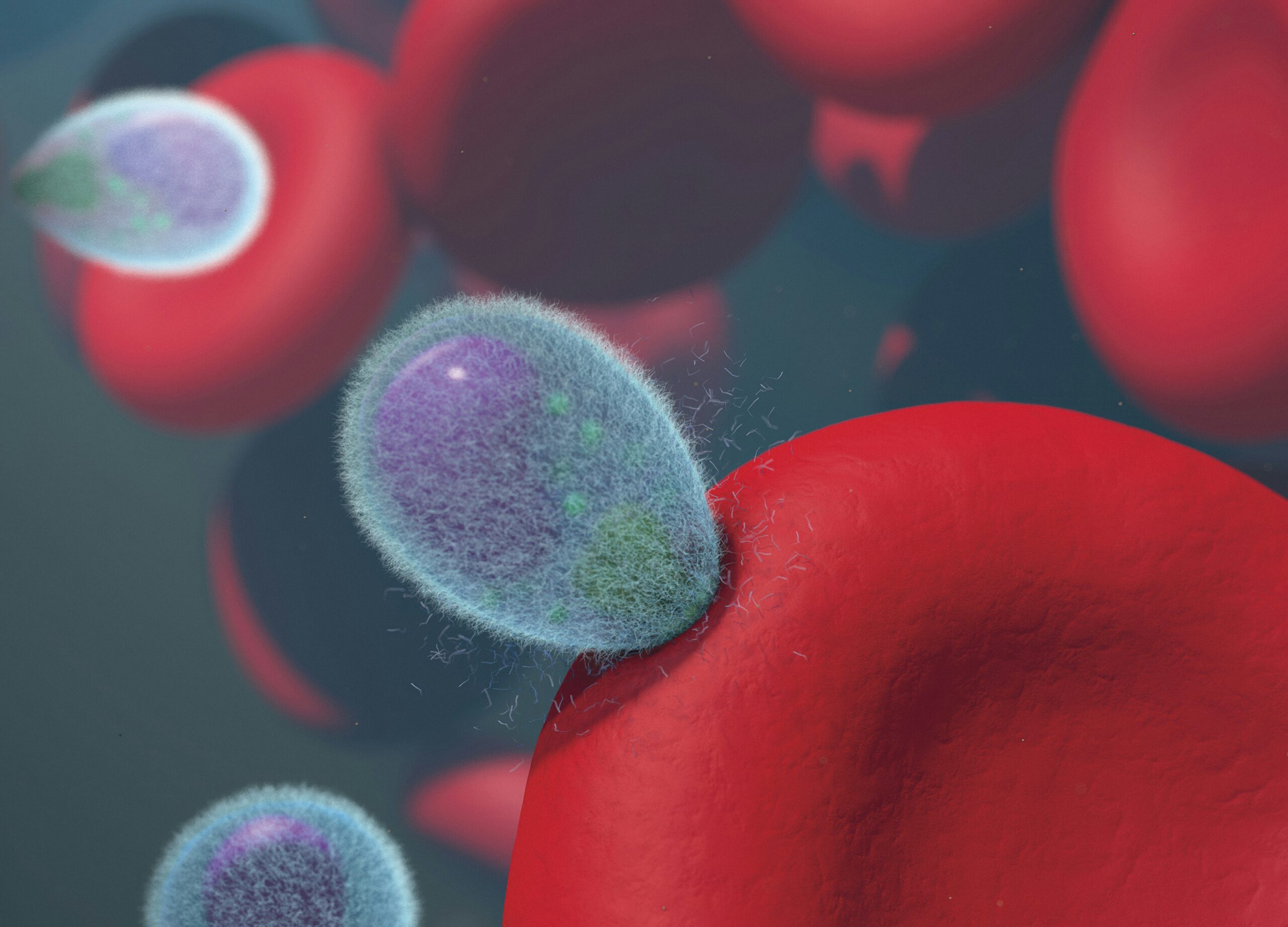
Image credit: Malaria Merozoites Invading Human Red Blood Cells Malaria merozoites (green/purple) invading human red blood cells (red). Merozoites are covered in a fuzzy coating of surface proteins (light blue) that are shed during invasion. Credit: NIAID https://www.flickr.com/photos/niaid/52845348454/